The Coronavirus pandemic has flooded media reports in recent weeks, with the reliability of information varying wildly. This poses challenges for health system leaders and facility managers: how do you communicate the right information to reassure patients and communities through the noise? As a community, we all have a role in finding the solution to this pandemic. With that in mind and as Array’s resident biocontainment design expert, I offer three strategies to help you set the minds of your patients and communities at ease.

1: Provide Context
Context cures misunderstanding, so let’s start by defining the risk posed by SARS-CoV-2 and the illness it causes, COVID-19. At the time of writing this article, SARS-CoV-2 had killed over 200 people in the US and over 10,000 people globally. By contrast, the flu has killed an estimated 20,000 – 52,000 people in the US alone from October 1st, 2019 to February 29th, 2020. That vast divide in impact speaks to the novelty of the disease. Where the flu is a certainty each year, routinely causing illness to over 30 million people, there are still many unknowns when it comes to COVID-19, which has affected over 250,000 people to date – the vast majority of whom are located outside the US. Considering these unknowns, recommending that concerned community members visit the CDC website, which is updated regularly, for accurate information on prevention and threat level is suggested.
Notably, approximately 80 percent of COVID-19 cases are mild and may not require medical attention. This is critical for communities to understand, as it helps prevent the collapse of healthcare systems by a flood of cases that do not require medical attention. The death rate is between 0.6% and 6.1% and is very dependent on how a country has handled COVID-19. Variances can be seen in countries such as Taiwan (very few cases, very low mortality), South Korea (many cases, low mortality), and Italy (many cases, high mortality). These discrepancies demonstrate show how the response to the pandemic will influence outcomes.

The Spread of COVID-19 and Telemedicine
The virus is believed to spread mainly from person-to-person contact. Most often, this spread happens as a result of close contact (about six feet). Person-to-person spread is thought to occur mainly via respiratory droplets produced when an infected person coughs or sneezes similar to how influenza and other respiratory pathogens spread. These droplets can land on nearby surfaces, then get transferred to the mouths or noses of people who are nearby or possibly be inhaled into the lungs. It’s currently unclear for how long the virus remains active on surfaces or objects – but CDC reports that the main cause of spread is thought to be person-to-person. Typically, with most respiratory viruses, people are thought to be most contagious when they are most symptomatic. The current recommendations of social distancing, hand washing, and covering coughs and sneezes are in place to reduce further spread of the virus.
Considering the way novel coronavirus spreads and that the majority of cases are mild, healthcare facilities should be advocating their telemedicine capabilities, according to the CDC. This remote care approach reduces the chances of infected patients transmitting the virus to healthcare workers and other patients seeking access to care and preserves access to in-person care for persons who are sicker. Health system leaders should also be working with the appropriate organizations to setup drive-through or at-home testing as the availability of testing begins to expand.
2: Highlight Healthcare Facility Preparedness
 Foremost, health systems should recognize that having plans is not enough. Hospitals need to increase the availability of tangible resources to prevent overrunning the healthcare system. For example, Italy’s healthcare system has been overwhelmed because they are running out of resources to take care of COVID-19 patients (oxygen, mechanical ventilators, medications). Some hospitals do not treat STEMIs, strokes or traumas anymore because they do not have the resources to do anything else but focus on COVID-19. There are anecdotes of family members having to manually ventilate patients because of the lack mechanical ventilators and staff are getting sick and overworked. Here in the US, strategic planners are projecting a shortage of ICU beds due to the pandemic. Earlier this week, Array Advisors released both a model to help health systems predict their bed capacity as well as a tool designed to help navigate initial surge capacity planning.
Foremost, health systems should recognize that having plans is not enough. Hospitals need to increase the availability of tangible resources to prevent overrunning the healthcare system. For example, Italy’s healthcare system has been overwhelmed because they are running out of resources to take care of COVID-19 patients (oxygen, mechanical ventilators, medications). Some hospitals do not treat STEMIs, strokes or traumas anymore because they do not have the resources to do anything else but focus on COVID-19. There are anecdotes of family members having to manually ventilate patients because of the lack mechanical ventilators and staff are getting sick and overworked. Here in the US, strategic planners are projecting a shortage of ICU beds due to the pandemic. Earlier this week, Array Advisors released both a model to help health systems predict their bed capacity as well as a tool designed to help navigate initial surge capacity planning.
That said, communicating to patients and communities to that your health system is prepared to help prevent spread of the virus remains useful, and it begins with demonstrating an understanding of CDC guidance. With that in mind, calling attention to CDC’s preparedness checklist and how your preparedness plan aligns with its requirements can help set minds at ease. That preparedness statement might include, but not necessarily be limited to, the following:
- An overview of how your hospital is prepared to prevent spread of COVID-19.
- The existence of, or preparedness plan as it relates to, Airborne Infection Isolation Rooms (AIIRs). CDC indicates that persons under investigation or confirmed with COVID-19 should preferably be treated within an AIIRs.
- If your hospital does not contain AIIRs, what precautions have been taken to ensure standard examination rooms can safely accommodate patients. CDC recommends that treatment within a closed-door standard examination room only occur if the exhaust is not recirculated within the building without HEPA filtration.
- A care plan for a limited number of patients with confirmed or suspected COVID-19 as part of routine operations.
- A detailed accounting of the facility’s ability to accommodate telemedicine. Successful telemedicine infrastructure addresses ease of use by patients unfamiliar with technology, equity of patient access to telecommunication tools, and maintenance of safety, privacy, quality of care, and patient experience as would be seen for in-person care.
3: Call Attention to Governmental Action
Globally, Governments are taking action to curb the spread of COVID-19 and fund the development of new treatments, the purchase of medical supplies and the resources needed to facilitate preparedness. In the US specifically, an $8.3 billion emergency coronavirus spending package has been approved, of which $826 million has been allocated for the development of coronavirus vaccines, treatments and tests. COVID-19 has already been replicated in a lab, a precursor to developing a vaccine, although experts expect that we are still a year away from a safe vaccine.
In addition to calling attention to the funding and rigorous pursuit of treatments resulting from Governmental action, sharing the following information can also help set the minds of community members at ease:
- A plan to release expanded testing nationwide has been rolled out.
- Studies are being performed on how COVID-19 spreads to bolster containment efforts.
- CDC has issued more than 23 guidance statements covering infection control, hospital preparedness assessments, personal protective equipment supply planning, and more.
- Travel restrictions have been imposed for citizens going to the countries most affected by the virus. Strict screening at airports is taking place, where incoming passengers are monitored for any signs or symptoms of illness. Incoming travelers from high-risk areas are triaged and quarantined.
By focusing on the vigilance, funding and expert guidance resulting from governmental action, health systems can help quell panic and reinstate appropriate levels of caution and confidence.
Design Matters
Designing communications that put COVID-19 in perspective, showcase your system’s preparedness, and call attention to governmental action are key to curbing undue panic. To get that message out effectively, consider taking advantage of CDC’s communication resources, leveraging video (which the brain processes 60,000 times faster than text), and using email effectively to strengthen lines of communication with your team.
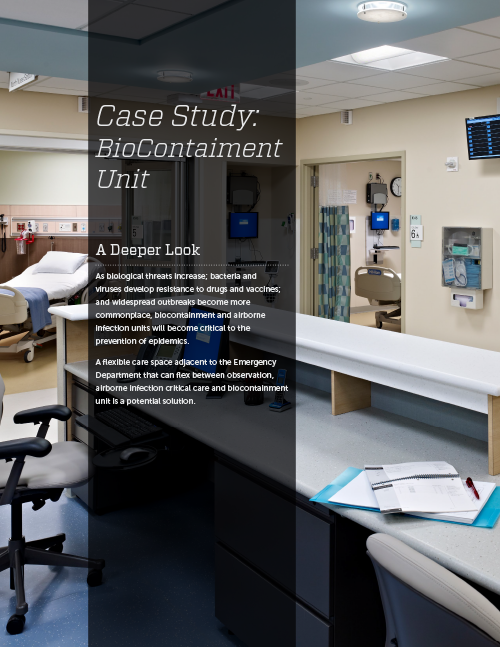
Similarly, ensuring that the design of your facilities meet the requirements necessary for safe treatment and containment of COVID-19 is essential. If adding additional AIIRs, keep in mind that While COVID-19 is capturing the attention of our nation today, it will not last forever. Modular or mobile units can provide short-term, temporary patient care facilities. More long term, a patient unit designed to alternately serve various patient acuities as well as infectious disease types (whether that’s for observation, med/surg, airborne infection isolation, or biocontainment) can provide the flexible operational preparedness hospitals need post COVID-19. Our team at Array mocked up a design that achieves this level of flexibility at HITT Contracting’s Co|Lab this fall. Explore that design by reading our case study on this topic.
This article was authored by Isabelle Arnold, a former employee of Array.




