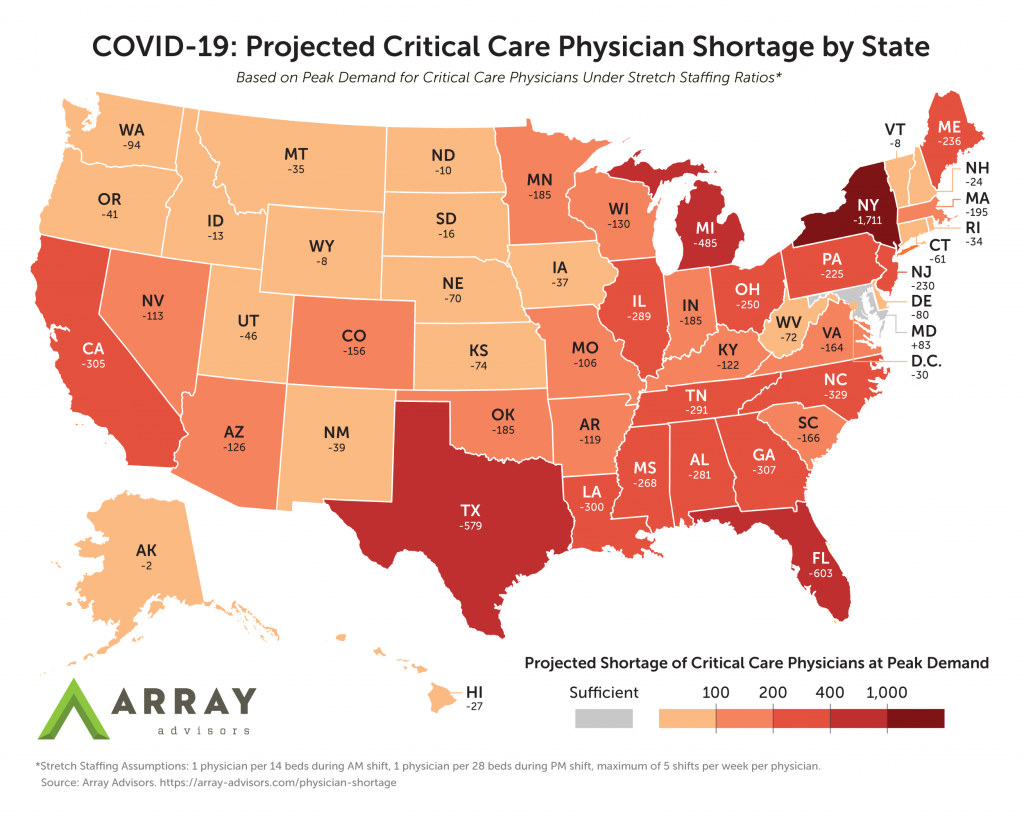
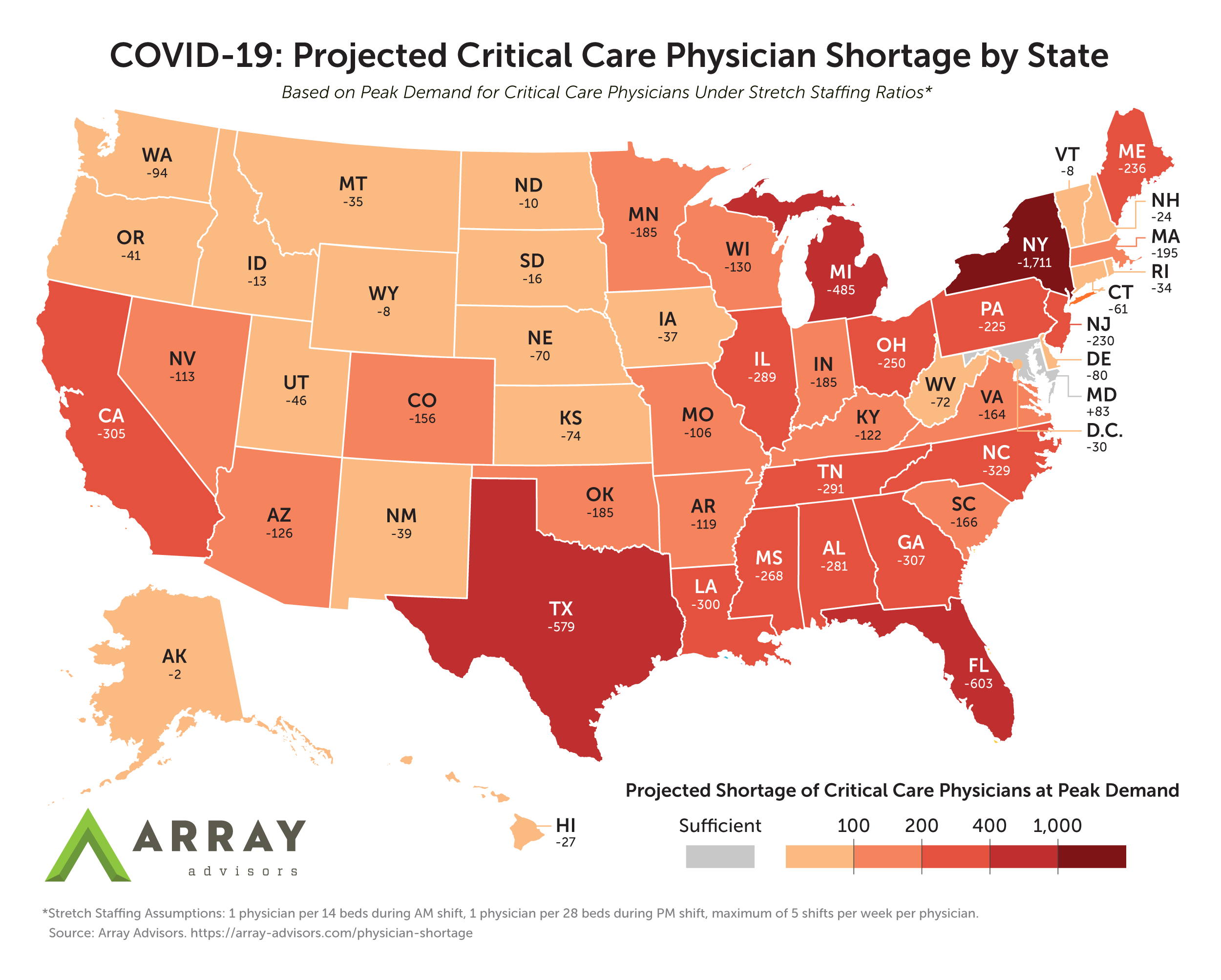
Most States Will Face Dramatic Shortages of Critical Care Physicians Even if Additional ICU Beds and Ventilators are Built
Washington, DC – At the national scale, the U.S. is projected to experience a shortage of over 7,900 critical care physicians due to COVID-19, according to new model from Array Advisors. The model projects the net demand for critical care physicians in each state as a result of COVID-19, accounting for both the projected demand for ICU beds and the potential reduction in providers due to infection of the healthcare workforce.
The shortage is expected at the projected peak of demand for critical care if the recommended ratio of one intensivist for every 14 ICU beds is maintained during the day. The state-level projections, which account for each state’s unique number of physicians and demand for ICU beds at the projected peak, overwhelmingly point to shortages. With the sole exception of Maryland, all states and the District of Columbia are expected to experience deficits, with the majority requiring 50 to 300 additional critical care physicians to meet the expected demand. Hard-hit New York is projected to experience a shortage of over 1,700 critical care physicians – more than three times their existing supply.
Download the model and results. Physician data provided by Pivotal.
As health systems across the country scramble to make room for the anticipated surge of COVID-19 patients, many efforts have been made to expand the supply of ICU beds. Unlike med-surg beds, there are no elective cases in the ICU that can be cancelled to make more beds available. But the creation of physical beds is only the first of many bottlenecks; even if health systems are able to add beds, they will need sufficient critical care physicians to staff them. The expected infection rate of the healthcare workforce further aggravates the problem by putting physicians out of commission. Array’s model assumes that as much as 10 percent of all critical care medical staff could be infected and thus unavailable at any given time.
“While the public attention has been on beds and ventilators, we must not lose sight of the staff needed to serve the coming influx of patients,” said Neil Carpenter, strategic planning VP at Array Advisors. “We need a national conversation about how to support and leverage our existing expertise, as well as how to contend with the coming surge of COVID-19 positive providers. In this fight, we need every provider to be well enough to work.”
Hospitals facing a potential shortage of critical care physicians will have limited options for ensuring coverage of ICU beds. Given the results of the model, sharing of critical care physicians between states will be an extremely challenging exercise in timing, if not altogether impossible. It may still be feasible to strategically deploy reserve medics to the areas with the highest need and transfer them as demand wanes, for as long as the “curves” across the country do not approach their peaks at the same time.
Even if the United States is fortunate enough to avoid a confluence of demand curves, hospitals will still have to find other ways to close the gaps. The following options will undoubtedly come with significant risk, but health systems and governing bodies may have no choice but to take them:
- Allow physicians with active COVID-19 to return to work and provide care via tele-ICU or directly to patients, if appropriate Personal Protective Equipment (PPE) is available
- Permit physicians who have only completed one year of their critical care fellowship to work independently
- Waive U.S. licensing rules to allow additional international tele-ICU coverage and scale existing operations abroad
- Recruit retired critical care physicians to re-enter the workforce
- Rapidly deploy artificial intelligence in conjunction with additional physician extenders to better leverage the existing critical care workforce
- Consider alternate standards of care for patients with extremely poor prognoses
The healthcare industry needs innovative solutions to battle the unprecedented coronavirus pandemic. Array Advisors, Array Analytics, and Array Architects will continue to provide ideas, design, and data-informed tools to help support their clients on the front lines of caring for our nation. For more tools from Array, visit our COVID-19 Resource Hub.
Study FAQ
Updated 4/1/2020. Since the publication of our model and results, we have received feedback and clarifying questions from a number of readers. To continue the conversation, we are sharing our responses publicly below and will continue to add any others as we receive them.
How did you define “Critical Care Physicians” in your model?
The physician counts in our Pivotal tool are sourced from the National Plan & Provider Enumeration System (NPPES). We selected providers with Medicare Provider Type “Physician/Internal Medicine” and a “Critical Care Medicine” specialization (taxonomy code: 207RC0200X) as their primary taxonomy.
Does your model account for the demand in ICU care not related to COVID-19?
Yes. We assumed the baseline demand for ICU coverage would remain the same and that COVID-19 patients would create new demand.
While most COVID-19 patients will require care outside of the ICU, we assumed that care will be provided by other physicians. In other words, our model does not assume that Critical Care Physicians will be needed to cover any other type of bed/setting for COVID-19 patients or any other patients.
Are there other specialists that can provide coverage in the ICU in lieu of a Critical Care Physician?
Some health systems do have other specialists with critical care expertise (such as pulmonologists) in addition to their fellowship-trained critical care intensivists. These specialists may be able to rotate and help cover ICU beds as peak demand hits different hospitals within a service area. This option is most likely feasible at Academic Medical Centers, but most community hospitals will not have that bench to draw from.
Can systems look to Advanced Practice Providers (APPs) to cover the shortage gap?
Critical care advanced practice practitioners are routinely used to care for critically ill patients, typically under the supervision of an intensivist. Baseline staffing models vary by state and even by hospital. During this crisis, we are hopeful that stretching of these models will be possible to meet demand. The Society of Critical Care Medicine has published one potential “crisis model” for tiered staffing that would depend heavily on the use of teams led by a critical care APP and a non-ICU physicians to enable each Critical Care Physician to oversee the care of a much larger group of patients.
In some states, such as Florida, scope of practice bills have been signed into law that allow nurse practitioners to work more independently. This will enable physicians who are now needed in the ICU or anywhere else in the hospital to be backfilled by these advanced practitioners, who in turn can over care for patients without COVID-19 or perhaps even low-acuity COVID-19 patients.
About Array
Recognized as a leader in healthcare facility design, consulting and technology, Array offers knowledge-based, data-informed services, including planning, architecture, interior design, transformation and asset advisory services. Using Lean as a foundation for a unique process-led approach, Array’s deliverables use data and technology to leverage real-time patient and real estate market trends required by today’s healthcare organizations. The company’s devotion to a healthcare-exclusive practice springs from the belief in the power of design and technology to improve patient outcomes, maximize operational efficiencies, and increase staff satisfaction.
Media Contact
Craig Meaney
Communications Manager
610-755-6488
@ArrayArch
cmeaney@array-architects.com
Note: a previous version of this release incorrectly stated that the projected shortage of critical care physicians at a national scale was 4,000.