In a previous lifetime, I worked for a large architecture firm that provided rollout retail work. While I cannot say that I particularly enjoyed this type of work very much, I did learn a lesson that would shape my career. This firm had achieved tremendous growth in the time I was there; and in a discussion with the president, he explained the success. They acquired a firm that focused on lean operations and ergonomics. The expertise this firm brought to the design process allowed us to save our clients money on staffing and workers’ compensation costs. To paraphrase the president, “If you can affect a business’ operations, then you can significantly affect their profitability.”
When I made the jump to healthcare architecture, I learned quickly how this mantra was very true. To understand the impact of design, you must understand the full spectrum of your clients’ business and operations. Too often, architects have been merely concerned with spatial aspects of the building, with some focusing too much effort on the aesthetics of the facility. Now I am as geeked about design as the next architect, however if a design does little to add to an organization’s business viability, then it has not provided value.
While doing some research on Life Cycle costs for healthcare facilities, I came across a graphic that made me laugh. It showed an iceberg with the tip protruding above the water, and the rest below sea level. The very top of the tip was colored blue with a 2% designation and the word “Design.” Although there was no other text, I knew exactly what the graphic was saying because I had seen this information portrayed in a myriad of ways. This image was showing that design composed only 2% of the Life Cycle costs for a building. Although I knew this to be a fact, for some reason this graphic made this point much more clear.
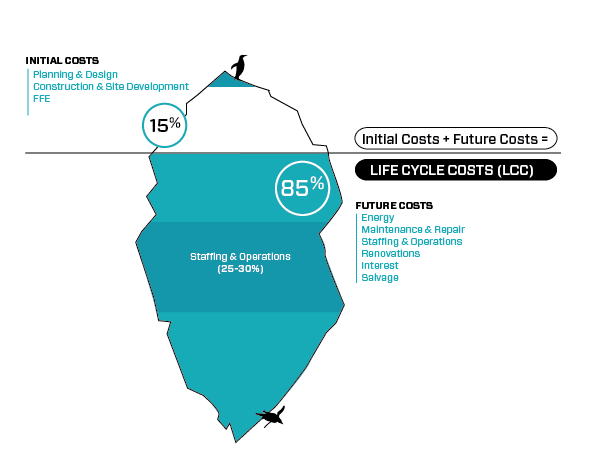
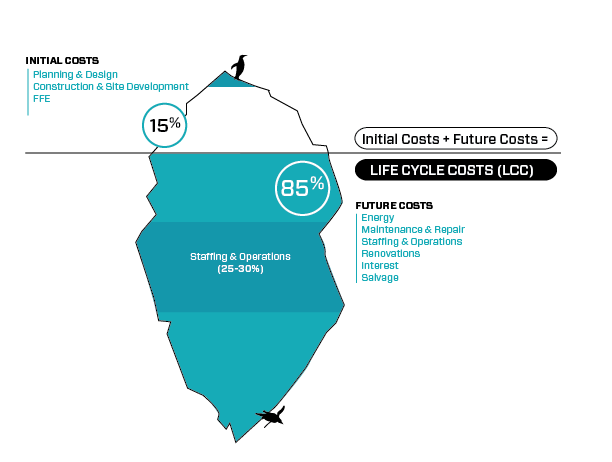
While this graphic may be perceived as mild plagiarism, I modified it to demonstrate my point, by adding the other components to represent all the Life Cycle costs of a medical building. Do an internet search on Life Cycle costs for any building and you will find an array of images that depict these components in various ways (pie charts, stacked charts, etc.) In my diagram, you can see that the physical built (visible) environment makes up about 15% of the Life Cycle costs of that building. (For you purists – I do realize that a true iceberg has mass density 0.917 g/cm³, so that 91.7% lies below the water surface – just roll with me as I make this point.)
The initial costs compose most of what can be seen (planning, design, construction, medical equipment, etc). However, the bulk of expenses for a hospital (or any building) occur after it is occupied. These include such items as future costs, energy, maintenance and repair, financing and mechanical costs, renovations, interest and salvage, with a major part being staffing and operations. (According to my research, staffing expenses alone account for approximately 50% of a hospital’s expenses.)
Many people understand how the design team can affect the physical plant and the mechanical portions of a building, but what about that operational function which composes some 25-30% of Life Cycle costs? How does your design team influence the operations of a healthcare organization? Below are some of the ways Array Architects is strategically affecting the bottom line of their client’s business.
Simulation Modeling allows users to adjust variables specific to the healthcare system, and observe the impact of the changes, providing insight into the most efficient and appropriate use of staff and space.
Lean Operations – By evaluating each process and every task for its effectiveness as part of the overall process flow, we can affect operational efficiency, effective care delivery and bottom-line value. Array believes so firmly in this process, that we incorporate Lean design principals on every project and utilize Kaizen events for our own in-office management.
Best Practice Metrics – Architecture and the built environment can and should support best practice medicine and clinical outcomes. From planning to interiors, from construction to completion, design teams must understand that the design of a facility will influence how staff provide services.
Increasing focus on interior design and the healing environment not only ensures the creation of beautiful spaces, but also helps clients realize their full potential to drive a change in culture, improve patient outcomes, increase patient satisfaction and foster a collaborative environment.
Facility Condition Assessments help define the existing building characteristics as a reference point for organizations to form an understanding of their real estate changes and/or needs.
To recap, I believe architects are not doing their clients justice when they do not fully invest in understanding the client mission, values and culture. The healthcare industry is at a crossroads with implementing ACA edicts, tackling population health and many other initiatives – they need their trusted advisors to be true stakeholders in their success.
Blog authored by Andy Vogel, a former principal with Array.




