As healthcare providers continue to identify the adjustments required to succeed in the new reality created by healthcare reform, one universal constant has been the need to increase operational process efficiency.
As any Healthcare CEO will attest, all of the planning and design efforts (not to mention dollars) that go into creating efficient built environments that support effective processes is for naught if their staff is not willing to embrace the methods needed to realize their potential. Training caregivers and support staff in efficiency processes is an ongoing commitment that the majority of leading providers have fully committed to – not just to cut costs, but because of the clinical outcome and patient satisfaction improvements that result.
However, providers shouldn’t be leading this charge alone – educators can take a leading role in preparing caregivers to instinctually think in these terms to ensure that effective and affordable healthcare is universally available (as mandated by the AHA). Perhaps the most effective tool available to educators is the Simulation Center.
In addition to teaching procedural techniques, when the audio-visual recording functions of Simulation Centers are paired with real-time location tracking equipment, they can become the perfect vehicle for testing actual performance against a pre-planned ideal model – providing near instant feedback to identify process faults and the practice environment to eliminate them.
Additionally, the close relationship that most educators have with local healthcare providers means that these facilities can be mutually beneficial – the needs of healthcare providers can help inform the curriculum while improving real-world skills in students, thus yielding better care delivery. This symbiotic relationship can create a spirit of collaboration that should be the hallmark of the healthcare industry.
When contemplating the addition of a Simulation Center to your core curriculum, educators should understand and align a few fundamentals in order to maximize benefits:
What are your priorities?
What level of realism is right for you?
How should your process flows be organized?
Which method of observation best supports your teaching techniques?
What is your communication strategy?
What is your long-range plan to accommodate industry changes?
How can a Simulation Center enhance your brand?
In this post, the first of three, I will address the first two questions which are more philosophical and overarching in nature. Your direction and responses to these questions will impact the design of the Simulation Center significantly.
What are your priorities? Understanding and aligning your teaching methodologies, student volumes, technological capabilities, and budgetary constraints will serve to ensure that the Simulation Center supports your mission rather than dictating it.
What level of realism is right for you? For students to effectively translate simulated learning to actual practice, the laboratory environment should be as realistic as feasible. Realism allows students to experience and practice their role in various scenarios and settings so that best practices for procedural processes, patient safety and interaction become instinctual – a more realistic simulation lab allows newly trained caregivers to transition from the teaching environment to a real hospital setting with ease. The temptation to create the highest level of realism should be balanced against budgetary, technology and spatial constraints. The balance between these constraints usually leads to one of these common scenarios:
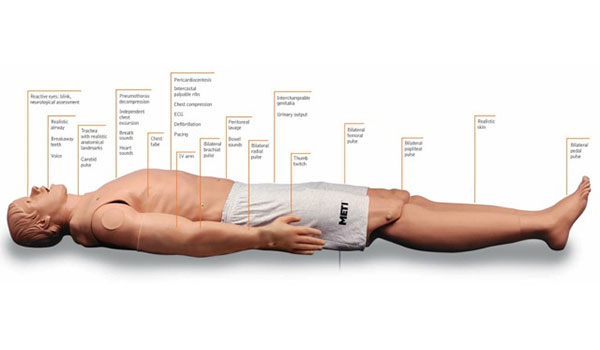
- Minimum Realism is consistent with the most basic general skills lab containing a group of beds/stretchers equipped with medium or low fidelity mannequins.
- Maximum Realism creates multiple “real” rooms (such as an Exam Room, OR, ED Treatment Bay, LDR, ICU, Inpatient Beds, etc.) complete with furniture, equipment and medical gases. This strategy can be extended to encompass support areas such as charting areas or medication rooms to simulate the entire care environment.
- Virtual Realism replaces “real” rooms with an immersive virtual environment (CAVE) that can be changed to simulate multiple scenarios. This scenario is most often used when space is scarce but funding and technology support is adequate.
An additional, and to some the most important, consideration is the use of standardized patients (i.e. actors playing the role of patients in mock-procedures). Their use increases the sense of realism when compared to mannequins; however they also have a significant impact on spatial requirements, departmental process flows, functional segregation, schedules and operational budgets.
In my second post, I will take a more in-depth look at specific elements of the Simulation Lab.
Continue to Part 2 of 3 Here.





