Recently engaged to design a new Dialysis Unit for a large New York City Hospital, Array approached the client to see if they would be open to us observing clinicians in the workspace to gain an understanding of how they deliver care, with a particular focus on the patient turnover process from an outpatient to inpatient shift.
Understanding how the client operates is an important first step that healthcare designers need to accomplish prior to designing a space that can support their workflow and processes. In many cases, the results are eye opening for both the designer and client and the insights gained will inform the design and possibly the way clinicians do their work.
Lean Design at a Glance:
At the root of Lean Design is the goal of achieving the Ideal State. The fundamental question being, “How close to ideal can one get?” Ideal Statein Lean Design is defined as a process or operation that is defect-free, that provides exactly what a patient needs, exactly as requested, in a timely manner, while creating no waste and in a safe environment.
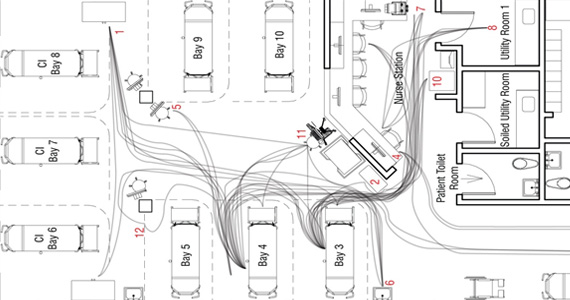
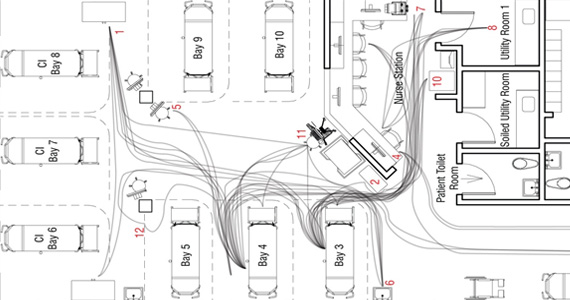
To reach an Ideal State, the first step in Lean Design is to effectively analyze and understand the Current State, i.e. the process as it currently exists. A valuable tool in Lean Design is direct observation. In this particular case study, we shadowed a Registered Nurse (RN) from a point in time when an outpatient was finished with their dialysis treatment, through turnover, to the start of a new inpatient treatment process (roughly a two-hour window). During this time, we were recording the RN’s actions step-by-step, assigning time segments to each action as well as spaghetti diagramming her movements.
A note when conducting observations for the first time: it is very important that the observed person feels comfortable and that they understand that you’re observing their processes and not their work habits. Also encourage them to speak up when they find themselves encountering a roadblock that requires them to clarify, document or search for supplies or personnel. In many cases, people develop a ‘work-around’ to a problem they encounter on a routine basis. These situations can be habit-forming and lead to unproductive and time-wasting actions.
A few interesting discoveries from our observation:
• Excessive wait times developed before a patient was first seen, due to inefficient patient turnover and lack of waiting space.
• Charts were not complete due in large part because the patient had not signed the consent form.
• Storage areas for supplies were scattered around the Unit, resulting in excessive footsteps.
• The inpatient required a catheter placement that should have been performed in their room prior to dialysis.
A valuable tool a healthcare designer can use to analyze an existing unit for inefficiencies in the layout is a spaghetti diagram. Since this particular case study is not very large, a manual diagram worked well. In more complex and larger units, technology such as a staff tracking wrist band can be worn and the data downloaded onto a computer system will map the clinician’s footsteps.
Some valuable insights learned from the spaghetti diagram:
• The existing Unit does not have proper space clearances around Treatment Bay 3 and it became a bottle neck on the Unit as staff needed to access a computer on wheels.
• A utility room is located off the Unit and added excessive footsteps.
• There is not a patient nourishment station, so the clinician needed to go to the staff lounge for necessary items.
• Necessary supplies are not at the patient’s bedside, two main supply cabinets are centrally located, however the location is not always convenient to the staff.
• There is one charting station per two patients (aligns with the RN-to-patient ratio), however these workstations are not at the bedside, which results in unnecessary transcription on paper to entering the information into the computer.
Although not every one of these situations may be indicative of what occurs for every patient, it certainly highlighted some existing process and unit design issues that can be improved upon on the new unit. Using our observation notes and spaghetti diagrams, we developed a Future State map i.e., a diagram that illustrates a more efficient process to administering a dialysis treatment. Although it’s not always possible to achieve an Ideal State, there are some important lessons that can be learned that would improve efficiencies in delivering patient care and if followed, can result in better patient care, higher satisfaction ratings and less caregiver stress.
A few important improvements in the Future State map included:
• Patient chart and blood sample results are ready and accessible to the RN.
• RN spends more time greeting patient and discussing their treatment.
• Dialysis tubing and necessary supplies are prepped and ready on a tray at patient bedside.
• Utilizing beds that have integral scales eliminates the need to do patient transfers.
• Each treatment bay has bedside charting so the RN does not need to transcribe vitals more than one time, eliminating the potential for an error and saving time.
In conclusion, conducting this exercise was an important first step in the process of designing the new Dialysis Unit. It highlighted issues in both the layout of the space and in some of the existing processes, which served as a valuable tool to help us understand the work processes. In designing the new Unit, we will work closely with the clinicians to provide adequate space and supply the necessary systems to achieve an Ideal State to support their daily tasks and provide superior care to their patients.





Beautiful sketch, I love the organic circulation flow and how it forms/informs the layout.