The role of Industrial Engineers does not traditionally involve work in the architecture or healthcare industries. Presently, however, given the high rate of healthcare costs in America, the industry is experimenting with a marriage of process engineers and architects to create more cost-effective environments with higher quality care. One recent example of architectural optimization in healthcare was conducted under the auspices of Array Architects for a large outpatient surgery center in the southeastern United States. To accommodate a growing volume of patients, this health system is going to open several satellite facilities across the country, testing a smaller community-focused model that would serve as a template for their growth. These smaller facilities will require a set amount of pre-operative care spaces (PRE-OP), post-anesthesia care spaces (PACU), and other necessary support areas to function. This study centered on the use of discrete event simulation modeling for layout and process planning purposes.
When architects are designing new healthcare facilities, they typically follow accepted design guidelines and client recommendations regarding the amount of space necessary in a specific facility. Due to the space utilization of the current facility, Array and the client were both interested in challenging these conventional guidelines by designing a space that most efficiently and precisely matched their specific function. In addition to this alternative space plan, the client was also interested in altering the current patient flow to improve the patient experience. In the current system, patients are transferred from Stage I recovery rooms to discharge recliners (Stage II) as they transition through the levels of recovery. The newly proposed model would allow the patient to fully recover in the PACU, with family members present, without moving to another location. The challenge would be to accommodate patients in the PACU for the duration of their recovery without causing backup in the ORs. These requests were translated into two major goals: 1) establishing an adequate number of recovery and PRE-OP rooms necessary to support the new patient recovery configuration without adding patient waiting time and 2) determining whether the space was large enough to support future growth in the form of an additional surgeon and patients. As a simulation model would be the best tool for finding a solution to this problem, Array engaged their healthcare systems engineer to study solutions.
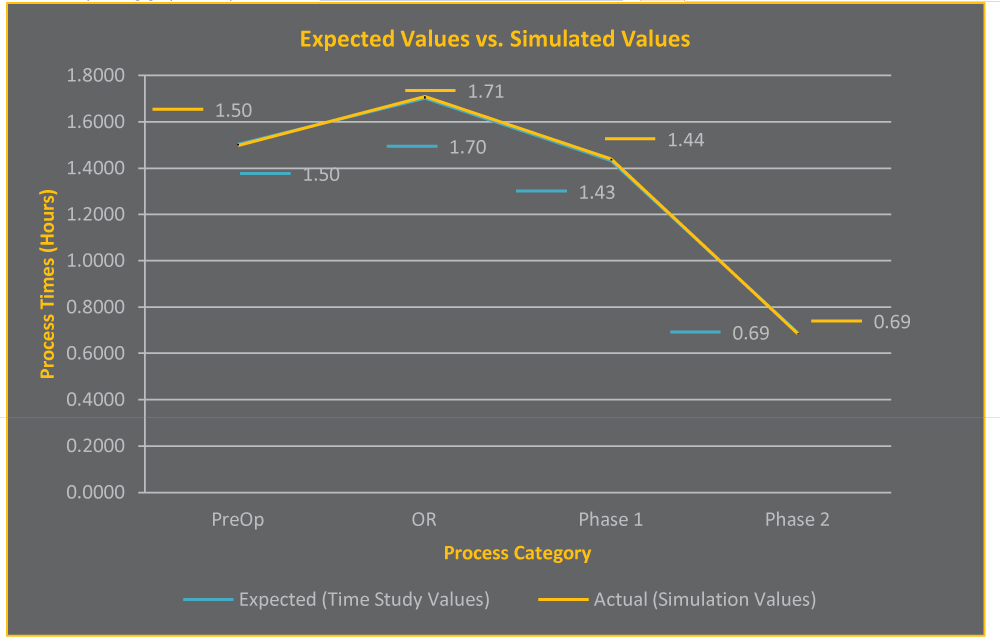
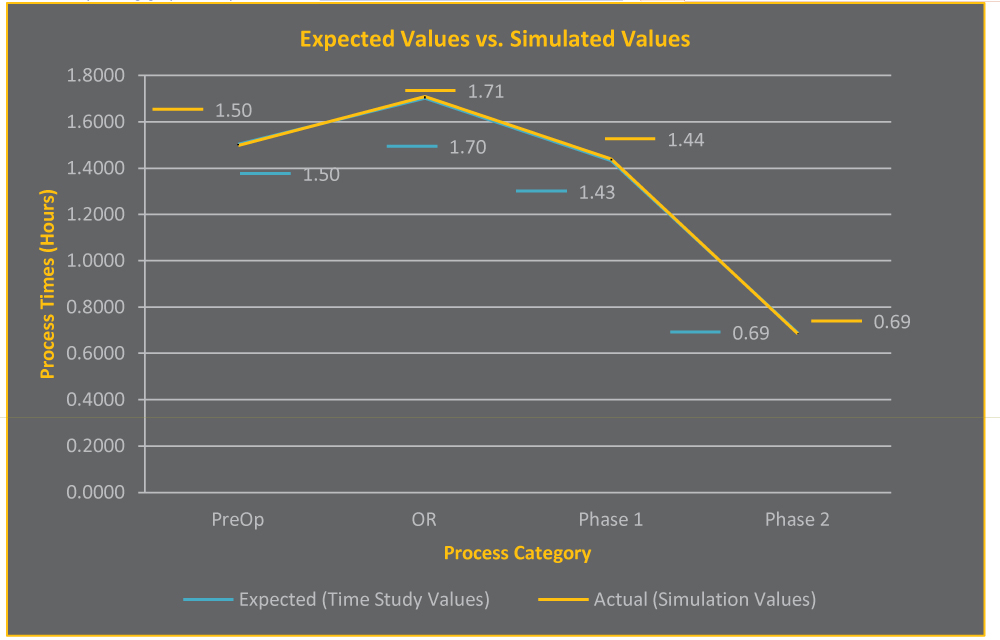
The key aspects of a simulation model are the data it runs on and its ability to accurately represent the parts of the system that relate directly to the project goals. Direct visual observations of the current work flow was arranged to validate the existing process map provided by Array and speak with front-line employees from the headquarters facility. Process time data compiled from a previous time study performed at the headquarters facility was used to generate distributions that powered the simulation. These process times were combined with the process map to create a simulation model using Arena Simulation software. To ensure the accuracy of the model, a paired-t confidence test was administered, in addition to other methods of validation and verification. It turned out that the actual values and the simulated values were almost perfectly correlated, resulting in 99.95% confidence that no statistically significant difference existed between the simulated and actual data, as can be seen in Figure 1. From this, it could be concluded that the processes in the simulated model were running almost exactly the same as the processes at the actual healthcare facility.
Once the simulation model was accurately representing the actual system, small changes could be made to see how they would impact the system. The simulation model was reconstructed for three different patient recovery scenarios — complete recovery in PACU with no overflow; complete recovery in PACU with overflow directly from surgery to PRE-OP; and complete recovery in PACU with overflow from PACU to discharge chair for phase two recovery. Each of these PACU overflow scenarios was paired with one of three options which tested the capacity limits of the surgery center, including adding a recovery room, adding a surgeon, and adding a recovery room and a surgeon.
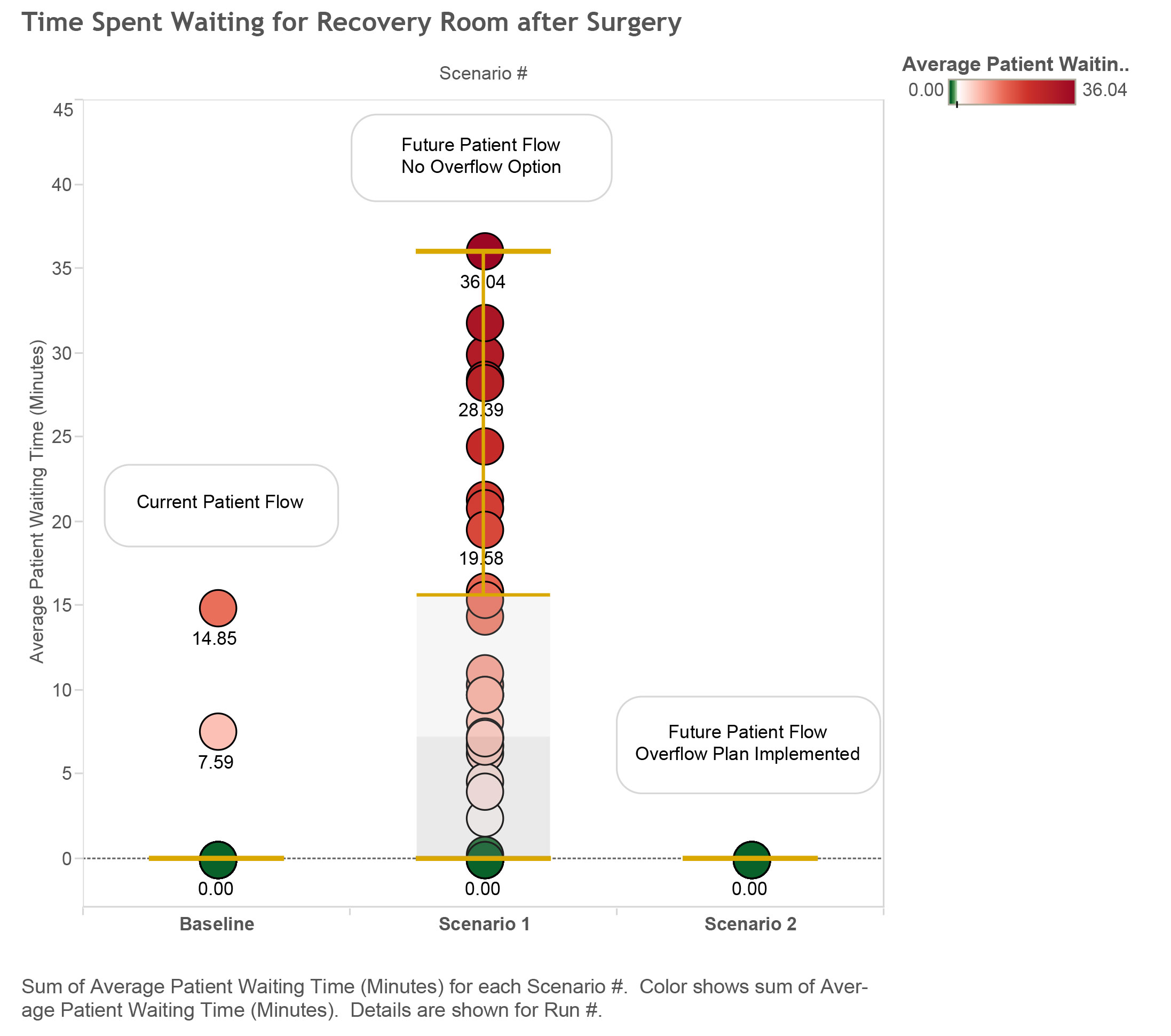
After modeling each of the scenarios combined with all of the options, output data was analyzed and it was determined that the desired future state Array proposed could indeed be achieved. In the ideal future operating state, patients recover fully in the PACU and a patient would never be required to wait for a recovery room to become vacant. The combination of scenarios and options that best meets these criteria allows complete recovery in the PACU with patients moving from surgery directly into a PRE-OP room when all recovery rooms are occupied. This solution leads to an improved patient experience, a more effective use of surgery center space, and a decrease in patient waiting times. According to the standard ratio of recovery rooms to operating rooms, there should be six recovery rooms and extra room for discharging patients. The proposed design solution suggests four recovery rooms are adequate. In the current operating state, on average, patients will wait 30 seconds after surgery before being placed in a recovery room. If the altered process was applied to the same layout, on average, every patient would wait 9.9 minutes, with a maximum average of 36 minutes per patient. The final solution requires that the PRE-OP rooms be used for recovery in case of a full PACU, which led to a 0 minute wait for patients exiting the operating room. The simulation model was used to test these different options and scenarios. Careful output analysis resulted in choosing a model with an efficient patient flow plan that involves zero waiting time after surgery and meets both goals set by the client.
While the results of the simulation prove viability of the proposed solution, we recognize that other factors contribute to a care model’s effectiveness. More rigorous prototyping and simulation modeling might study the areas of maximum patient capacity, ideal scheduling, personnel utilization, and cost analysis, to definitively determine the most efficacious operational scheme for the health institution. Nevertheless, the work conducted by Array for the surgery center is a prime example of the way systems engineering and architecture can come together to help the healthcare industry function more efficiently.
Ready for more? Read additional blogs on event simulation and simulation modeling.




